When a SARS-CoV-2 particle meets a human cell, it’s the virus’s spike proteins that begin the work of invasion. If you’ve seen the image of the novel coronavirus, the one drawn by medical illustrators at the CDC, you’ll know these proteins as the red protrusions that stud the gray blob, like radioactive trees on a rocky planet. The spike proteins latch onto receptors at the surface of the host cell. Once locked into place, they fuse the virus’s membrane with the host cell’s membrane. The break-in complete, the virus proceeds to deposit its genetic material in the cell, which instructs the cell’s machinery to produce more copies of the virus.
Fortunately, the novel coronavirus is as dumb as it is vain. Some viruses elude vaccine developers because they make little typos in their genetic code as they replicate, effectively disguising them from antibodies on the prowl. SARS-CoV-2, however, has a proofreading enzyme that limits such shifty mutations. In other words, the enemy is mostly stable and knowable, the easiest kind to defeat. More than 50 vaccines are in clinical trials on humans now, all of them designed to induce antibodies that can attach to and neutralize the spike proteins.
Two vaccine candidates appear to have pulled this off. Last week, Pfizer and its German development partner BioNTech announced interim results from their late-stage clinical trial, which showed their vaccine to be more than 90 percent effective (a later analysis pushed that to 95 percent). On Monday, the biotech company Moderna released similarly impressive results from trials of the vaccine it's developing in partnership with the National Institutes of Health.
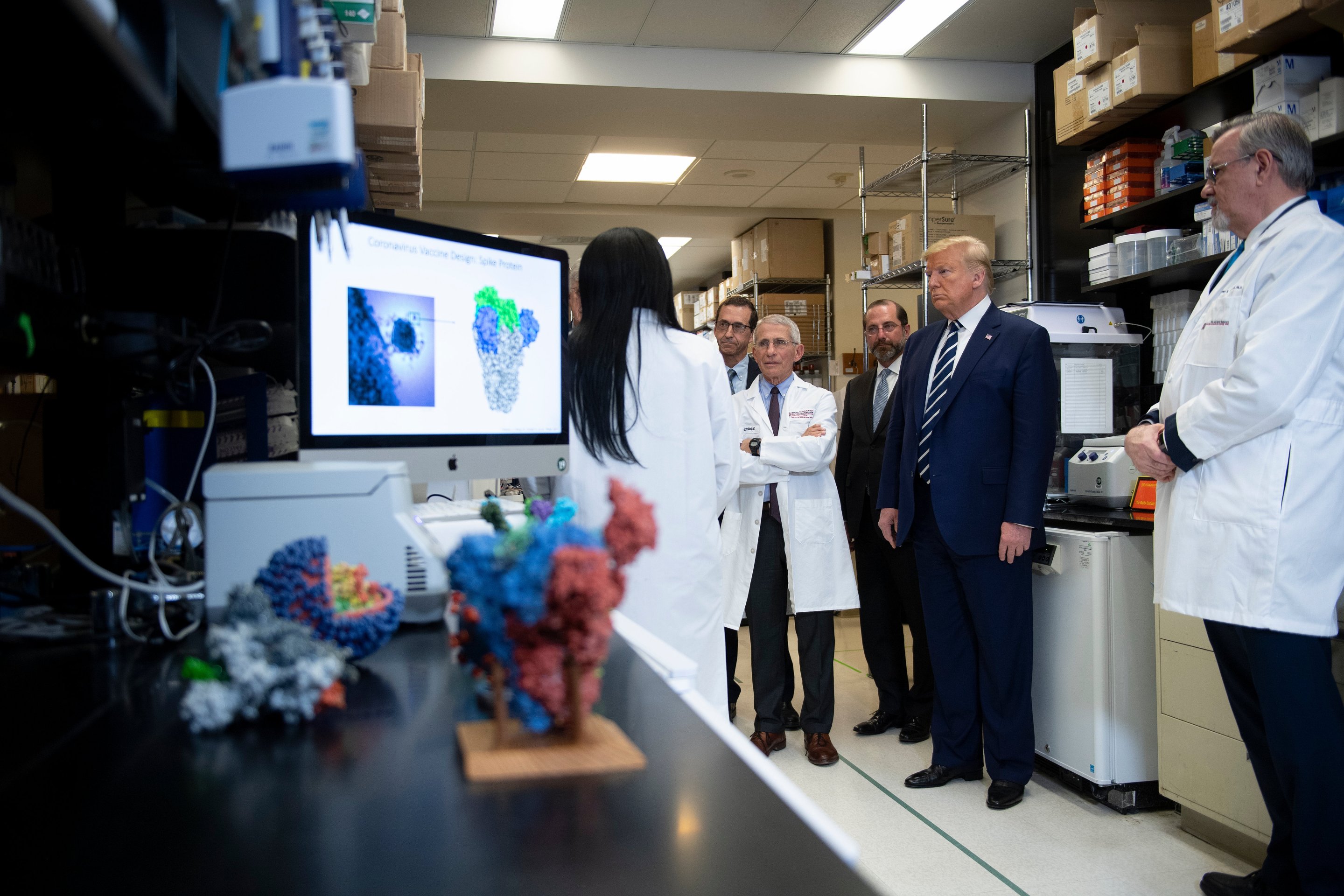
Skepticism toward pharmaceutical company press releases is natural and perfectly understandable; it may help to think of the announcements as data check-ins, performed by fully independent data safety and monitoring boards, which review the trial data at pre-established intervals and before anyone at the companies can. (In Moderna's case, the independent board includes members from Health and Human Services' Biomedical Advanced Research and Development Authority, and from the National Institute of Allergy and Infectious Diseases, the NIH institute run by Anthony Fauci.)
The rapid, destructive spread of COVID-19 in the U.S. has had the perverse effect of speeding these trials up. The Moderna study protocol, for example, initially scheduled the first interim analysis to take place when the trial group hit 53 positive cases. But by the time the board could review the data, there were 95 infections in the trial group, nearly two-thirds of the 151 needed to complete the trial. Of those first 95 people in the study who tested positive for COVID-19, 90 were in the placebo group (that is, they had not received the vaccine). The data gathering isn't finished, and any evidence will be submitted to the FDA for review, but the preliminary results, as Fauci put it, are "truly striking."
A favorite exercise in both biotechnology and partisan politics is desperate angling for credit, especially when the accomplishments are as striking and as desperately needed as these. Republicans, those famous champions of big government, called the Moderna and Pfizer vaccines triumphs of the Trump administration and Operation Warp Speed, the federal government's vaccine development and distribution initiative. Trump, for his part, could not decide whether the vaccine news was a testament to his administration or a conspiracy against it.
Was the timing intentional? Pfizer CEO Albert Bourla had said weeks before the election that Pfizer would be submitting its data to the FDA in the third week of November, but a report in MIT Technology Review suggests it's possible he'd been urged to commit to that timeline by scientists concerned Trump might pressure the FDA to rush through approval before the election.
Warp Speed puts Democrats in an awkward political position, too. How does one rightfully criticize the federal government's handling of the COVID-19 crisis without undermining already low public confidence in vaccines, which a Biden administration will have to distribute? Or decry Trump's dangerous habit of demanding political favors from independent agencies without suggesting the scientists who work at those agencies have actually succumbed to his pressures? For New York Governor Andrew Cuomo, the answer was: not so tactfully. “The first question is 'Is the vaccine safe?'" he said in a September press conference. "Frankly, I'm not going to trust the federal government's opinion.”
Cuomo's comments make clear the fallout of the last four years: A sizable portion of the country has been conditioned to reflexively distrust anything associated with Trump, just in time for a moment that demands trust in a government he happens to run. To the extent that any government activity occurring between Jan. 21, 2017 and Jan. 21, 2021 is Trump's doing, Operation Warp Speed happened on his watch. But it would be wrong to call it a distinct achievement of the Trump administration, and just as wrong to consider it something poisoned by his name being on the letterhead.
Jason Schwartz, an assistant professor of health policy at Yale's School of Public Health, told me Operation Warp Speed was probably the type of program an administration of either party would launch. Goofy name aside, Warp Speed's core functions are sensible enough: to fund research and development of vaccine candidates; to attenuate the risk of vaccine development by purchasing doses in advance; and to coordinate vaccine distribution strategy with the help of government logistics experts. So far, the initiative is working well, Schwartz said, because it's supplemented and not supplanted "the tried and true ways that we have to evaluate vaccines and to recommend their use." (So you can give Trump credit, if you like, for not getting in their way.)
Pfizer troubled Trump's story by offering its own answer to the credit question: “We were never part of the Warp Speed,” Pfizer’s head of vaccine research and development Kathrin Jansen told the New York Times. “We have never taken any money from the U.S. government, or from anyone.” As Republicans were quick to point out, because they love and value the public sector, that was not entirely true. Pfizer didn't take money from the U.S. government to fund research and development, but it did receive a commitment from the government in July to purchase at least $1.95 billion of doses of a successful vaccine.
Advance purchase agreements are a critical feature of an initiative like Warp Speed. Developing vaccines, Schwartz explained, is an expensive undertaking for pharmaceutical companies, and certainly less lucrative than focusing on drugs that millions of people may end up taking every day. "[Warp Speed] took that financial calculus out of vaccine manufacturers' decision-making because the financial risk was absorbed by the federal government," he said.
In just a week after the Pfizer announcement, the importance of the Warp Speed commitment became clear: Moderna announced that its vaccine is as effective as Pfizer's and doesn't require the ultra-cold chain storage Pfizer's does. That's the sort of competitive disadvantage that would be bad for business—and bad for the motivation to undertake development in the first place—had the government not already guaranteed the Pfizer vaccine a market.
Like the Moderna vaccine, the Pfizer vaccine also relies on publicly funded research. The SARS-CoV-2 spike proteins shift shape as they fuse the viral and host cell membranes, and it's easier for antibodies to respond to them when the proteins are in their pre-fusion shape. In 2017, scientists at the NIH's Vaccine Research Center and the University of Texas–Austin figured out how to mutate the spike protein in a way that could stabilize the pre-fusion shape. That mutation is now encoded in Pfizer's vaccine. “Make no mistake, this was done in academic and government labs,” Dan Leahy, the chair of the university's molecular biosciences department, told CBS Austin last week.
Of course, Pfizer's version of events plays much better on TV. “I wanted to liberate our scientists from any bureaucracy. When you get money from someone, that always comes with strings,” Bourla said on Face the Nation, asked why the company had not taken Warp Speed research and development money. “And also, I wanted to keep Pfizer out of politics, by the way.” Read that in the simplest, shallowest way, as a rebuke of the Trump administration, or recognize it for the sort of private-sector vanity that precedes Trump and will long outlast him.
Here’s that moment when @pfizer’s @AlbertBourla told @margbrennan why he said “no” to taxpayer dollars: “I wanted to liberate our scientists from any bureaucracy” pic.twitter.com/IJ7QVQkKAp https://t.co/HXkPHTXNQ2
— Face The Nation (@FaceTheNation) November 9, 2020
The economist Mariana Mazzucato has written about the false distinction canny CEOs like to draw between government lethargy and private-sector dynamism. Bourla's is one of many self-fulfilling eulogies for government competence. "The story has been used to downsize the state through an increased number of public activities being outsourced to the more 'dynamic and efficient' private sector, chopping away at the very brains of the state," Mazzucato writes in her book The Entrepreneurial State.
Mazzucato writes that the challenge of a state that fosters innovation is to ensure that any public-private relationships it enters are symbiotic rather than parasitic. That's an especially important consideration now given the equitable access issues wrapped up in vaccine distribution, where a lack of transparency in Warp Speed contracts is some cause for some concern. "We know so little about pricing," Schwartz said. "We have these press releases of these bulk orders that the government has committed to purchasing from manufacturers—the prices, even among those, sort of vary per dose. We don't know how long those agreements last. We don't know whether the government has a stake in assuring affordable pricing."
The work of the Biden administration, then, is to improve transparency and regain public trust at a time when faith in government to meaningfully improve anything may well be nearing extinction. This will be slow and painstaking work, but so much that has led to this point has been slow and painstaking.
Eureka moments—Newtons plunked by falling apples—linger in the popular imagination, but a more typical story of science drags and meanders. "'Could you build a career on coronaviruses?' was really a question in 2010,” one virologist told STAT in February. He described a grant proposal he wrote a decade ago: “I spent half of the first page—maybe three-quarters of the first page—justifying why we still worked on SARS.”
The new vaccine candidates are the result of years of unglamorous basic science research and hard-fought battles for funding. If that truth lacks the narrative excitement “Warp Speed” suggests, that doesn’t make it any less inspiring. The news of the last two weeks is a reminder that the money and brainpower needed to solve monumental problems have always been at our disposal. Public investment can pay off even when the state seems irreparably disassembled, even when the politicians in charge are hostile to the idea that government might do good. In these lowest and stupidest of times, here, finally, is some occasion for hope.